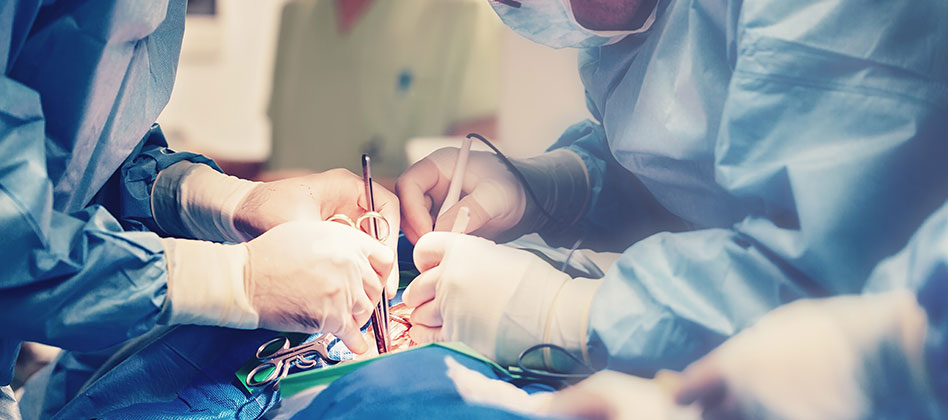
Emergency laparotomy is a major surgical procedure, with 30,000 to 50,000 performed every year in the UK. However, around 15% of patients are reported to die within 30 days of surgery. Over 25% of patients remain in hospital for more than 20 days after surgery, costing the NHS over £200m a year.
Funded by the Health Foundation, the Emergency Laparotomy Collaborative (ELC) was established in 2015 to use a quality improvement (QI) approach to tackle this. The ELC initially brought together 28 hospitals and 24 NHS trusts across 3 AHSN regions: Kent Surrey Sussex; Wessex; and West of England.
The ELC worked to improve standards of care for patients undergoing emergency laparotomy surgery, reduce mortality rates, complications and hospital length of stay, while encouraging a culture of collaboration and embedding QI skills to ensure sustainability of change.
This involved the spread and adoption of the evidence-based Emergency Laparotomy Pathway Quality Improvement Care (ELPQuiC) bundle within the NHS trusts. The programme has brought together dozens of staff at collaborative learning events from across the trusts – from emergency departments, radiology, acute admission units, theatres, anaesthetics and intensive care.
Through roll-out of the care bundle across 28 hospitals, the project has successfully reduced lengths of hospital stay by an average of 1.3 days, and crude mortality rates have fallen by 11%. In Kent Surrey Sussex alone, it is estimated that 66 lives have been saved since the project began.
A health economics analysis suggests every £1 spent will result in approximately £4.50 benefit to the wider health and social economy.







 +44 (0)300 303 8660
+44 (0)300 303 8660
 enquiries@kssahsn.net
enquiries@kssahsn.net
 @kssahsn
@kssahsn